Patent Ductus Arteriosus (PDA)
What is it?
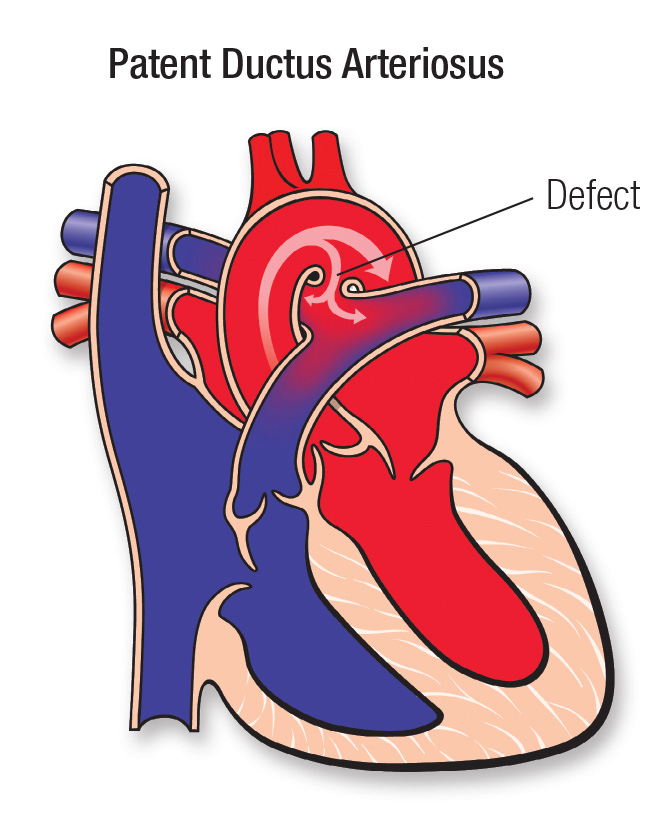
An unclosed hole in the main body artery (aorta).
Before a baby is born, the fetus's blood does not need to go to the lungs to get oxygenated. The ductus arteriosus is a hole that allows the blood to skip the circulation to the lungs. However, when the baby is born, the blood must receive oxygen in the lungs and this hole is supposed to close. If the ductus arteriosus is still open (or patent) the blood may skip this necessary step of circulation. The open hole is called the patent ductus arteriosus.
More information for parents of children with PDA
What causes it?
The ductus arteriosus is a normal fetal artery connecting the aorta and the main lung artery (pulmonary artery). The ductus allows blood to detour away from the lungs before birth.
Every baby is born with a ductus arteriosus. After birth, the opening is no longer needed and it usually narrows and closes within the first few days.
Sometimes, the ductus doesn't close after birth. Failure of the ductus to close is common in premature infants but rare in full-term babies. In most children, the cause of PDA isn't known. Some children can have other heart defects along with the PDA.
How does it affect the heart?
Normally the heart's left side only pumps blood to the body, and the right side only pumps blood to the lungs. In a child with PDA, extra blood gets pumped from the body artery (aorta) into the lung (pulmonary) arteries. If the PDA is large, the extra blood being pumped into the lung arteries makes the heart and lungs work harder and the lungs can become congested.
How does the PDA affect my child?
If the PDA is small, it won't cause symptoms because the heart and lungs don't have to work harder. The only abnormal finding may be a distinctive type of murmur (noise heard with a stethoscope).
If the PDA is large, the child may breathe faster and harder than normal. Infants may have trouble feeding and growing at a normal rate. Symptoms may not occur until several weeks after birth. High pressure may occur in the blood vessels in the lungs because more blood than normal is being pumped there. Over time this may cause permanent damage to the lung blood vessels.
What can be done about the PDA?
If the PDA (ductus) is small, it doesn't make the heart and lungs work harder. Surgery and other treatments may not be needed. Small PDAs often close on their own within the first few months of life.
Most children can have the PDA closed by inserting catheters (long thin tubes) into the blood vessels in the leg to reach the heart and the PDA, and a device can be inserted through the catheters into the PDA like a plug. The figure below on the left shows one example of how a catheterization is used to close the ductus. If surgery is needed, an incision is made in the left side of the chest, between the ribs. The ductus is closed by tying it with suture (thread-like material) or by permanently placing a small metal clip around the ductus to squeeze it closed. If there's no other heart defect, this restores your child's circulation to normal. In premature newborn babies, medicine can often help the ductus close. After the first few weeks of life, medicine won't work as well to close the ductus and surgery may be required.

What activities can my child do?
If the PDA is small, or if it has been closed with catheterization or surgery, your child may not need any special precautions regarding physical activity and may be able to participate in normal activities without increased risk.
As far as follow up in the future, depending on the type of PDA closure, your child's pediatric cardiologist may examine it periodically to look for uncommon problems. The long-term outlook is excellent, and usually no medicines and no additional surgery or catheterization are needed.
Congenital Heart Defect ID sheet
More information for adults with PDA
What causes it?
The ductus arteriosus is a normal fetal artery connecting the main body artery (aorta) and the main lung artery (pulmonary artery). The ductus allows blood to detour away from the lungs before birth.
Every baby is born with a ductus arteriosus. After birth, the opening is no longer needed and it usually narrows and closes within the first few days of life.
Sometimes the ductus doesn't close after birth. Failure of the ductus to close is common in premature infants but rare in full-term babies, and the cause is usually not known. Some patients can have other heart defects along with the PDA.
How does it affect the heart?
Normally the heart's left side only pumps blood to the body, and the right side only pumps blood to the lungs. In a person with PDA, extra blood gets pumped from the body artery (aorta) into the lung (pulmonary) arteries. If the PDA is large, the extra blood being pumped into the lung arteries makes the heart and lungs work harder and the lungs can become congested.
How does the PDA affect me?
If the PDA is small, it won't cause symptoms or problems because the blood flow and pressure in the heart and lungs aren't changed appreciably from normal. The only abnormal finding may be a distinctive type of murmur (noise heard with a stethoscope), sometimes called a "machinery" murmur.
If the PDA is large, breathlessness may be due to reduced heart function or problems related to high pressures in the lungs. High pressure may occur in the lung vessels because more blood than normal is being pumped there. Over time this may cause permanent damage to the lung blood vessels (pulmonary hypertension).
What if the defect is still present? Should it be repaired in adulthood?
If the PDA is small, it doesn't have to be closed because it doesn't make the heart and lungs work harder.
Patients with a moderate- or large-sized PDA may develop problems related to the increased blood flow to the lungs. These patients may have improvement if the PDA is closed. Closing the PDA can now usually be performed by catheter coil placement or other device insertion to plug the abnormal communication (referred to as interventional or therapeutic catheterization.)
Surgery may be the best treatment option for some patients. The surgeon doesn't have to open the heart to fix the PDA. An incision is made in the left side of the chest, between the ribs. The PDA is closed by tying it with suture (thread-like material) or by permanently placing a small metal clip around the PDA to squeeze it closed. Occasionally in the adult, a surgical patch is used. If there's no other heart defect, this restores the circulation to normal.

If I still have a PDA, what activities can I do?
If the PDA is small, or if the PDA has been closed with catheterization or surgery, you may not need any special restrictions and may be able to participate in normal activities without increased risk.
Patients with moderate or large PDAs and patients with pulmonary hypertension may need to restrict activity. They should discuss this with their cardiologist.
Ongoing Care
What will I need in the future?
Depending on the type of PDA closure, your cardiologist may examine it periodically to look for uncommon problems. The long-term outlook is excellent, and usually no medicines and no additional surgery or catheterization are needed.
Medical Follow-up
Patients with a small PDA need periodic follow-up with a cardiologist. Patients with a PDA that's been successfully closed rarely require long-term cardiology follow-up unless there's additional cardiac disease. Only rarely will they need to take medicine after surgical or device closure. Your cardiologist can monitor you with noninvasive tests if needed.
Activity Restrictions
Most patients with a small unrepaired PDA or a repaired PDA don't need any special precautions and can participate in normal activities without increased risk. After surgery or catheter closure, your cardiologist may advise some limitations on your physical activity for a short time even if there's no pulmonary hypertension.
Exercise restriction is recommended for patients with pulmonary hypertension related to PDA.
Endocarditis Prevention
Endocarditis prophylaxis is generally not needed more than six months after PDA device closure. However, endocarditis prophylaxis is recommended for PDA patients with a history of endocarditis, for those with prosthetic valve material and for unrepaired PDA with associated pulmonary hypertension and cyanosis. See the section on endocarditis for more information.
Pregnancy
Unless there's pulmonary hypertension or signs of heart failure, pregnancy is low risk in patients with PDA.
Will You Need More Surgery?
Once a PDA has been closed, it's unlikely that more surgery will be needed. Rarely, a patient may have a residual hole. Whether it will need to be closed depends on its size.






