Unstable Angina
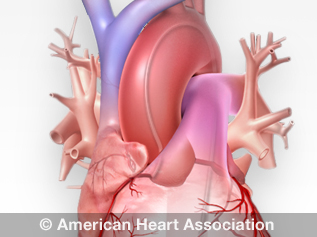
Unstable angina, one of several acute coronary syndromes, causes unexpected chest pain, and usually occurs while resting. The most common cause is reduced blood flow to the heart muscle because the coronary arteries are narrowed by fatty buildups (atherosclerosis) that can rupture, causing injury to the coronary blood vessel. This results in blood clotting, which blocks blood flow to the heart muscle.
Unstable angina should be treated as an emergency. If you have new, worsening or persistent chest discomfort, call 911 and go to the emergency room. You could be having a heart attack, increasing risk for severe cardiac arrhythmias or cardiac arrest, which could lead to sudden death.
Learn about an unstable form of angina called Prinzmetal angina.
Causes of Unstable Angina
Blood clots that block an artery partially or totally are what cause unstable angina. Typically, the artery will have plaque buildup (atherosclerosis) that has narrowed the vessel. The plaque may have damaged areas that make it easier for blood clots to form. Angina can occur each time a clot blocks blood flow in an artery. Learn more about excessive blood clotting.
Symptoms of Unstable Angina
Unstable angina pain or discomfort:
- May occur while you're resting, sleeping or with little physical exertion.
- Comes as a surprise.
- May last longer than stable angina
- Usually isn't relieved by rest or medicine.
- May get worse over time.
- Can lead to a heart attack.
Treatment for Unstable Angina
First, your health care team will need to find the blocked part or parts of the coronary arteries by performing a cardiac catheterization. In this procedure, a catheter is guided through an artery in the arm or leg and into the coronary arteries, then injected with a liquid dye through the catheter. High-speed X-ray movies record the course of the dye as it flows through the arteries, and blockages can be identified by tracing the flow. An evaluation of how well your heart is working also can be done during cardiac catheterization.
View an illustration of a cardiac catheterization(link opens in new window).
Next, based on the extent of the coronary artery blockage(s) your health care team will discuss with the following treatment options with you:
- Percutaneous coronary intervention (PCI) may be required to open a blocked coronary artery. This procedure involves undergoing cardiac catheterization, followed by using a catheter with a small inflatable balloon at the tip. The balloon is inflated, squeezing open the fatty plaque deposit in the inner lining of the coronary artery. Then, the balloon is deflated and the catheter is withdrawn. This procedure is often followed by insertion of a stent to keep the coronary artery vessel open to allow for improved blood flow to the heart muscle.
- Coronary artery bypass graft surgery may be necessary depending on the extent of coronary artery blockages and medical history. In this procedure, a blood vessel is used to route blood around the blocked part of the artery.
For more information, talk to your health care team.





