Tachycardia: Fast Heart Rate
Quick Facts
- The normal average resting heart rate is 60-100 beats per minute. Tachycardia is a resting heart rate over 100 beats per minute.
- Supraventricular tachycardia (SVT/PSVT) starts in the upper heart chambers.
- Sinus tachycardia starts from the heart’s natural pacemaker, the sinus node.
- Ventricular tachycardia (VT) begins in the heart’s lower chambers and can be life-threatening.
- Tachycardias are usually diagnosed by doing an electrocardiogram (EKG).
The normal average resting heart rate is 60-100 beats per minute. Tachycardia is when the heart beats too fast when at rest — at a rate of more than 100 beats per minute. This can depend on age, health status and physical condition. Learn about the types of tachycardias:
- Supraventricular tachycardia (SVT)/ Paroxysmal supraventricular tachycardia (PSVT)
- Sinus tachycardia
- Ventricular tachycardia
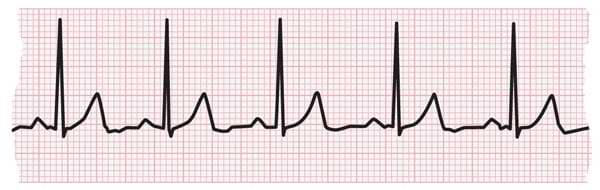
EKG strip showing a normal heartbeat

Supraventricular tachycardia (SVT)/ Paroxysmal supraventricular tachycardia (PSVT)
SVT is a fast heart rate, greater than 100 beats per minute, that starts in the atria, the heart’s upper chambers. The electrical signals occur abnormally and speed up the heart rate. The rapidly beating heart prevents the heart chambers from filling completely between contractions (beats). This may decrease blood flow to the body.
SVT is the most common abnormal heart rhythm in infants and children. Paroxysmal SVT means that the abnormal rhythm may come and go over minutes or days.
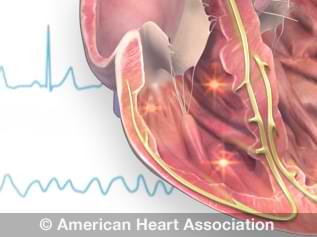
View an animation of tachycardia.
What are the risk factors for SVT/PSVT?
- Anxiety and stress
- Increasing age – people middle-aged and older
- Sex – women more than men
- Children (SVT is the most common abnormal heart rhythm in children)
For some people, SVT/PSVT is caused by exercise, stress or lack of sleep, while others do not notice anything at all.
Issues that may cause an SVT episode include:
- Age
- Anemia
- Heart disease
- Dehydration
- Coronary artery disease; having had heart surgery or other heart problems
- Congenital heart disease
- Other heart conditions, such as Wolff-Parkinson-White syndrome
- Chronic lung disease
- Excessive caffeine intake
- Excessive alcohol intake
- Smoking or other tobacco products
- Drug misuse, including cocaine and methamphetamines
- Pregnancy
- Menopause
- High blood pressure
- Certain over-the-counter medications, including those for asthma, colds and allergies
What are the symptoms of SVT/PSVT?
- Very fast (rapid) heartbeat that may come and go
- A fluttering or pounding in the chest (palpitations)
- A bounding pulse feeling in the neck
- Weakness or feeling very tired (fatigue)
- Chest discomfort
- Shortness of breath
- Lightheadedness or dizziness
- Sweating
- Fainting (syncope) or near fainting
- Nausea
How is SVT/PSVT diagnosed?
SVT
Your health care professional will ask you for a detailed medical history (including potential causes) and a list of symptoms. Then you will be advised to get an electrocardiogram (EKG).
PSVT
Because PSVT is “paroxysmal” (occasional and sudden), an EKG taken during an appointment may look normal. To “catch” an episode, your health care professional may suggest a portable heart monitor (Holter monitor or event monitor) to wear at home that will record your heart rhythm over time.
How is SVT/PSVT treated?
Most people with SVT/PSVT don't need treatment. However, an episode may be stopped with one of these methods, under the supervision of a health care professional. These affect the vagus nerve, which helps control the heartbeat.
- Carotid sinus massage: Gentle pressure is applied on the neck where the carotid artery splits into two branches.
- Vagal maneuvers: Simple moves such as coughing or holding your nostrils closed while attempting to blow air through your nose.
- Dive reflex: This is the response by the body to plunging your face in ice-cold water. This is called a vagal maneuver. It should be done only with a health care professional’s instruction.
Other treatments as needed:
- Medications: If you have frequent episodes of SVT, you may be prescribed medication to control your heart rate or restore a normal heart rhythm.
- Cardioversion: This procedure delivers a shock to the heart, through patches or paddles, to restore the normal heart rhythm.
- Catheter ablation: Thin, flexible tubes called catheters are inserted through the veins or arteries, usually in the groin. Sensors on the tip of the catheter use heat or cold energy to create tiny scars in the heart to block irregular electrical signals. This restores a normal heartbeat.
Living With My Imperfect Heart

My Life With a Turbocharged Ticker

Sinus Tachycardia
Sinus tachycardia is an increase in the heart rate. In this condition, the heart’s natural pacemaker, the sinus node, sends out electrical signals faster than usual.
The heart rate is faster than normal, but the heart beats properly. It’s a common response to exercise, but it’s concerning when it occurs at rest.
What causes sinus tachycardia?
A rapid heartbeat may be your body’s response to common conditions such as:
- Anxiety
- Fright
- Severe emotional distress
- Strenuous exercise
- Fever
- Some medications and illegal drugs
- Pain
Other, less common causes may include:
- Anemia
- Infection
- Increased thyroid activity
- Heart muscle damage from heart attack or heart failure
- Severe bleeding
- Very low blood pressure
- Lung disease
How is sinus tachycardia treated?
Your health care professional should consider and treat the cause of your sinus tachycardia, rather than just treating the condition. Simply slowing the heart rate could cause more harm if your rapid heartbeat is a symptom of a more serious or long-term problem.
Ventricular Tachycardia
Ventricular tachycardia (VT) is a fast heart rate that starts in the heart’s lower chambers (ventricles). Electrical signals in the heart’s lower chambers fire abnormally fast. This interferes with electrical impulses coming from the sinus node, the heart’s natural pacemaker.
The disruption results in a faster-than-normal heart rate. This rapid heartbeat keeps the heart’s chambers from filling completely between contractions, which reduces blood flow to the rest of the body.
VT may be either well-tolerated or life-threatening, requiring immediate diagnosis and treatment. The severity of VT depends largely on whether you have other heart conditions and the type of VT you have.
What causes ventricular tachycardia?
Ventricular tachycardia is most often associated with disorders that disrupt the heart’s electrical conduction system. These disorders can include:
- Lack of coronary artery blood flow, depriving oxygen to heart tissue
- Cardiomyopathy, distorting the heart’s structure
- Medication side effects
- Use of illegal drugs such as cocaine or methamphetamine
- Sarcoidosis, an inflammatory disease affecting skin or body tissues
- Abnormalities of the heart that result in scarring of heart tissue, sometimes called “structural heart disease”. The most common cause is a prior heart attack
- Congenital heart conditions, including long QT syndrome
- Imbalance of electrolytes needed for conducting electrical impulses
What are the symptoms of VT?
VT symptoms can vary. Common symptoms include:
- Dizziness
- Palpitations
- Shortness of breath
- Nausea
- Lightheadedness
- Fainting (syncope)
- Cardiac arrest, in extreme cases
- Chest pain
How is VT treated?
Treatment will depend on your symptoms and the cause of your VT. Possible treatments include:
- Medication that helps prevent arrhythmias
- Radiofrequency ablation, a procedure that destroys the cells causing the VT
- Surgery to implant a cardioverter defibrillator (ICD), which delivers an electrical pulse to the heart to reset a dangerously irregular heartbeat
- Immediate electrical defibrillation, in extreme cases
More resources:
- Exploring SVT: Resources for health care professionals
- Learn what the target and maximum heart rates are for people your age.