Other Heart Rhythm Disorders
Arrhythmias include many conditions such as bradycardias and tachycardias. Additional heart rhythm disorders are:
- Adams-Stokes Disease
- Atrial flutter
- Sick sinus syndrome
- Sinus arrhythmia
- Wolff-Parkinson-White Syndrome
Adams-Stokes Disease
Adams-Stokes Disease, also called Stokes-Adams disease, refers to a heart block or other arrhythmia that can slow the heart rate considerably, causing fainting (syncope) or convulsions. It’s caused when the heart’s electrical signals are interrupted as they pass from the upper (atria) to the lower (ventricles) chambers.
Atrial flutter
Atrial flutter occurs when rapidly firing electrical signals cause the muscles in the heart’s upper chambers (atria) to contract at a very rapid rate (250 to 350 times per minute). This leads to an overly fast heartbeat, which can have either a regular or irregular rhythm.
Atrial flutter is much less common than atrial fibrillation (AFib or AF), but its causes and consequences are similar. People with atrial flutter can also have periods of atrial fibrillation.
Symptoms of atrial flutter
Atrial flutter may present with a heartbeat that’s overly fast, irregular or with heart palpitations (feeling a hard, fast or irregular heartbeat in the chest). Other symptoms include:
- Fast, steady pulse
- Chest pain (angina)
- Shortness of breath
- Weakness
- Lightheadedness
- Fainting (syncope)
- Heart palpitations
- Irregular heart rhythm combined with AFib
- Stroke
If you have these symptoms and think you may have atrial flutter, contact your health care professional immediately.
Other conditions and risk factors
Atrial flutter is often associated with other conditions such as:
- Heart failure
- Previous heart attack
- Open-heart (bypass) surgery
- Heart valve surgery
- Valve abnormalities or congenital defects
- High blood pressure
- Atrial fibrillation
- Thyroid dysfunction
- Alcoholism (especially binge drinking)
- Chronic lung disease
- Diabetes
- Smoking
- Previous stroke
Learn more about atrial flutter.
Sick sinus syndrome
When the sinus node (also called the sinoatrial or SA node) doesn’t produce its electrical signals properly, the heart rate slows down, pauses or speeds up. This is referred to as sick sinus syndrome.
In this condition, the heart rate can change between an overly slow rate (bradycardia) and an overly fast rate (tachycardia).
Sinus arrhythmia
Common in children, this type of irregular heart rhythm refers to changes in the heart rate during breathing. The heart beats faster for a few moments when you breathe in. When you breathe out, it slows down. Sinus arrhythmia is normal.
Wolff-Parkinson-White Syndrome (WPW)
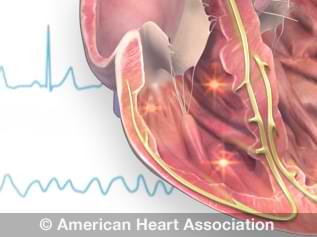
In this disorder, the electrical pathways between the heart’s upper (atria) and lower (ventricles) chambers malfunction. This allows electrical signals to reach the ventricles too early. Those electrical impulses can then be “bounced back” to the atria.
This can produce overly fast heart rates. Other people with WPW Syndrome may not feel any obvious symptoms but still face serious risk.
Some people with WPW also have atrial fibrillation.
Diagnosis and treatment
Your health care professional can detect WPW Syndrome through an electrocardiogram (EKG or ECG). This noninvasive test can show irregularities in your heart rhythm.
Your treatment plan will depend on many factors, including your risk of future arrhythmias as well as how frequent and severe your symptoms are. People who don’t have symptoms may not need treatment.
Possible treatment options for WPW Syndrome may include:
- Medications that regulate heart rhythm
- Cardioversion
- Ablation
- Open heart surgery
Ablation is the most common treatment for WPW Syndrome. It has a high success rate and a low risk of complications.