Where and how you sit matters when getting blood pressure taken at the doctor's office
By Laura Williamson, American Heart Association News

Millions of people with normal blood pressure may be misclassified as having blood pressure that is too high because of improper positioning when measurements are taken, new research suggests.
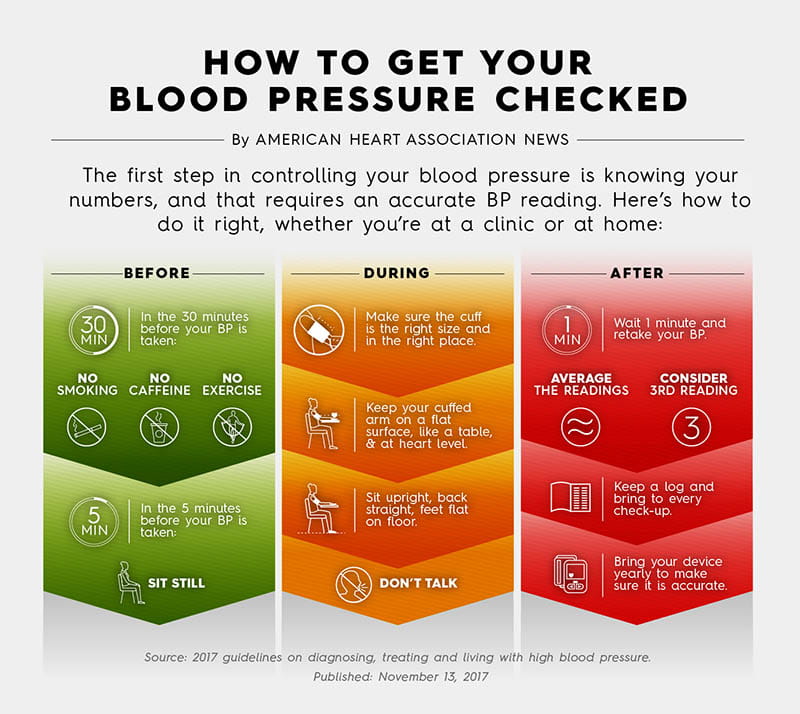
Guidelines from the American Heart Association and American College of Cardiology call for a patient to be seated in a chair with feet flat on the floor, their back supported and the arm wearing the blood pressure cuff supported at heart level. Doing so helps ensure an accurate reading. But many health care professionals take blood pressure measurements while the patient is seated on an examining table, leaving their legs to dangle and their back and arm unsupported.
"That's not conducive to taking blood pressure accurately," said researcher Dr. Randy Wexler, a primary care physician at The Ohio State University Wexner Medical Center in Columbus. He will present the research on Saturday at the AHA's Scientific Sessions conference in Philadelphia.
Being misclassified with high blood pressure, also called hypertension, can lead to "people undergoing treatment who don't need it," Wexler said. "People may not need to be on as much medication, which has side effects. That's where having good and accurate blood pressure measurements becomes important."
In the study, 150 adults were randomly assigned to one of three groups. In one group, blood pressure readings were taken on a fixed-height exam table and then in an exam chair with adjustable positioning. A second group had the same readings taken in reverse order. A third group had both sets of readings taken in the exam chair. There was a rest period before each set of readings. Results were pooled and the average of three measurements taken on the table were compared to the average of those taken in the chair.
For readings taken on the exam table, the average systolic (top number) blood pressure was 7 mmHg higher and the average diastolic (bottom number) reading was 4.5 mmHg higher than those taken seated in the chair, adhering to guideline-recommended positioning. The researchers concluded this difference was large enough to misclassify millions of people as having hypertension whose blood pressure was actually within the normal range.
"We were not surprised there was a difference," Wexler said. "We were surprised at how much of a difference there was." The findings were published in September in the journal eClinicalMedicine.
Nearly half of all U.S. adults are estimated to have high blood pressure. Hypertension is diagnosed when measurements consistently reach or exceed 130 mmHg systolic or 80 mmHg diastolic.
People given medication to lower blood pressure when they don't need it are at risk for pushing their blood pressure too low, a condition known as hypotension, said Dr. Jordana Cohen, a nephrologist at Penn Medicine in Philadelphia who was not involved in the new research. Low blood pressure can cause dizziness, lightheadedness and fainting and can lead to falls.
"We need to make sure we measure blood pressure correctly and treat it correctly," said Cohen, also an associate professor of medicine at the University of Pennsylvania. "Health systems need to prioritize this. We have to convince them it is economically smart to do so because it will lead to better outcomes."
Health care professionals see so many patients with so many chronic conditions that they often don't have enough time to take blood pressure measurements properly, Wexler said. Research suggests that primary care providers would need more than 26 hours per day to follow all preventive and chronic disease care guidelines for seeing patients, or more than nine hours per day when providing team-based care.
"We need to make things more efficient," said Wexler, adding that future research should look for such strategies. "But how do we make changes that are doable without slowing down the process of the visit?"
Find more news from Scientific Sessions.





