Scrambling to restart a stopped heart — when the patient is the president of the American Heart Association
By American Heart Association News
At 6:20 a.m. on Nov. 13, Dr. John Warner climbed off a stationary bike inside the Anaheim Convention Center and started walking across the street to his hotel.
It was a big day for Warner, part of a big week.
About 15,000 people from around the globe and from all aspects of cardiovascular medicine were in Anaheim, California, for the American Heart Association’s Scientific Sessions meeting. It’s the AHA equivalent of the Super Bowl and with Warner serving a one-year term as the organization’s volunteer president, he was essentially the starting quarterback.
The day before, he opened the conference by delivering a speech he’d been crafting for months. Today would be even more exciting. Next up was the major announcement of new guidelines for how doctors nationwide should treat high blood pressure, and later was his President’s Dinner.
At 6:37 a.m., Warner walked into his suite and found his wife, daughter and son scurrying to leave.
Lisa, Lauren and Jacob never join him at medical meetings, but his starring role made this the exception. They were free until the dinner, so they were headed to visit Pepperdine University, where Lauren, a high school senior, has applied. Their ride would be here in eight minutes and nobody was ready.
John grabbed a bottle of water from the refrigerator and sat on the sofa taking sips. Lauren walked by and he wished her well on the outing. She went to finish straightening her hair, he went to shower.
At 6:40 a.m., Lisa was brushing on blush in front of the bathroom mirror. John leaned back on the bed and checked email on his phone.
At 6:43 a.m., Lauren called 911. Her dad wasn’t breathing. He hadn’t been for two minutes.

***
The headline that spread across the internet went something like, “American Heart Association president suffers heart attack at heart meeting.”
This is the first time the details are being shared in print. The Warners and others involved spoke with American Heart Association News because of the larger story to be told.
At best, what happened underscores the tools and technology available when heart disease strikes. At worst, it underscores how much scientists and doctors still don’t know.
After all, if heart disease could sneak up on John Warner – a 52-year-old interventional cardiologist-turned-CEO of a hospital system who closely followed his heart health because his father and grandfather had bypass surgery in their 60s – then it can hit anyone at any time.
***
Lisa was about to put on eyeliner when she heard wheezing. She turned and saw John’s chest heaving.
She dashed to the bed and found his eyes frozen open, and he didn’t respond to her. Was this a heart attack? A seizure? She called the hotel operator to send help and screamed: “Lauren! Jacob! Come quick!”
The color of John’s face went from pink to blue, about that fast.
Jacob, a senior at Duke, checked John’s neck for a pulse. He couldn’t find one. At the same time, John gave a final breath. His chest refused to rise again.
Jacob and Lisa ran down the hall to find someone, anyone, who knew what to do. It clicked to Lisa that they were at Sessions and trained healthcare professionals were everywhere. She just didn’t know where.
Lauren, left alone with her dying dad, remembered watching an AHA Hands-Only CPR how-to video. She’d practiced giving chest compressions on a manikin and learned that the beat of “Stayin’ Alive” – about 100 per minute – was the right rate for those compressions.
She put one palm flat on the center of his chest, the other hand on top, and pushed down, over and over, hoping she was pushing hard enough. Fortunately, experts were on their way.
***
“We need a cardiologist!” Jacob screamed as he ran down the hall in bare feet, Lisa a few steps behind.
The door to a room they’d already passed flew open, drawing them back.
“We need help in my room,” Lisa said. “It’s John Warner.”

Lisa didn’t know the woman, Tia Raymond. But Tia knew John. Not just as the AHA president or as the head of UT Southwestern University Hospitals in her hometown of Dallas. He’s been her mother-in-law’s cardiologist for about 12 years. The day before, Tia and John chatted in the lobby.
Tia is a pediatric cardiologist in the intensive care unit at Medical City Children’s Hospital in Dallas. She was at Sessions to present research on the resuscitation of children who go into cardiac arrest in a hospital.
Before checking into the hotel, she went online and selected a room near the far end of the top floor because she’s a light sleeper. She wears earplugs, too, yet Jacob’s wails came through loud and clear.
Wearing her pajamas – her favorite Michigan football T-shirt and shorts – Tia followed Jacob to the end of the hall. Tia’s roommate, research nurse Janie Garza, searched for her shorts so she could join them.
***
Lauren had given about 30 compressions, enough for her wrists to ache, when Jacob and Tia rushed in.
Tia followed protocol by asking that someone call 911 and find an AED, an automated external defibrillator, a machine that can shock a fibrillating heart back into rhythm. She then went straight into giving compressions.
The mattress was springy, making compressions less effective. So Tia and Jacob lowered John to the floor. Janie entered as John’s body was being situated between the bed and a wall.
Oh my God,” Janie thought. “He’s so blue.”

Janie works for the Sarah Cannon Research Institute, but she’s been in emergency situations alongside Tia at Medical City for about 10 years. Like dance partners performing their signature routine, they snapped into action — Tia at John’s chest, giving compressions; Janie at the head, giving rescue breaths.
John's chest moved, so they knew the breaths were getting air into his lungs.
Tia’s untamed hair flopped in her face. She needed a hair tie. Jacob knew Lauren always wears one on her wrist, so he asked her for it. She flung a black band like a slingshot, landing it on John’s chest.
What Tia really needed was the AED. Jacob took off to find it. On his way out the front door, Kodie Hartman – a tall, muscular hotel security guard – came running in.
“The AED is on the way,” he said.
***
Tia continued pushing hard and fast on John’s chest, making sure each compression went deep enough. Better to break a rib and save his life than go too shallow and lose him.
She took turns with Kodie. His compressions were plenty forceful. Janie’s rescue breaths became more effective thanks to a mask inside a medical bag Kodie brought.

Finally, the machine arrived.
A digital voice told them to give compressions for 30 seconds, give two breaths and repeat for 2 minutes. The machine then checked the heart’s electrical activity to determine whether a shock was needed.
Back off, the machine announced, because a zap was coming in 3, 2 …
Lauren grabbed the crown of Lisa’s head and tilted her mom’s head down.
With her forehead on Lauren’s shoulder, Lisa couldn’t see what was happening. In a calm, confident voice, Lauren said: “Lord, we know you’re in control. You’ve got this. Lord, we ask you to be with these people and give Dad the care that he needs.”
***
Jacob paced, pondering a way to help.
A computer science major and future software engineer, he went into troubleshooting mode: What’s not being accounted for?
The ambulance! He could guide the EMTs to the room.
But, wait. Leaving might mean missing the most painful, pivotal moment of his life. He’d regret that forever. And there was maybe a 5 percent chance the EMTs needed him to lead the way.
Action beat inaction. Off he ran again, bare feet burning against the carpet.
***
John’s skin turned even darker blue. Janie felt him turn colder and sweaty.
The first shock failed to revive him.
“He’s doomed,” Tia thought as the AED began guiding them through another 2-minute cycle of CPR.
The machine told everyone to back off for another shock.
Lisa watched this time.
She stood with her hands over her face as if blowing warmth into them on a cold day. Peering over her fingers, she saw the burst of electricity jolt John into the air.
***
As the AED started a third round, Janie said, “The color in his face is getting better.” Tia agreed.
The machine deliberated a possible third jolt. The verdict came back: “No shock advised.”
The lifesavers began a fourth round of compressions. Janie gave a rescue breath. As she started another, John reached up to push her away.
Tia grabbed John’s other hand and felt his pulse. It was booming.
“We have a pulse!” she hollered. “WE HAVE A PULSE!”
Just then – still not yet 7 a.m. – Jacob and the EMTs burst in. Soon, John was being loaded onto a stretcher.
***
In basic terms, a clogged artery caused all this.
Cholesterol and cells (known as atherosclerotic plaque) had gradually narrowed an artery supplying the back of John’s heart, creating a partial blockage. A blood clot formed there, completely stopping the blood flow. This is a heart attack, the type called a “STEMI,” for ST elevation myocardial infarction. But not everyone who suffers a STEMI has their heart stop pumping.
Sometimes, as in John’s case, the plumbing problem triggers an electrical glitch known as ventricular fibrillation. In that abnormal rhythm, the heart doesn’t pump blood effectively — a cardiac arrest. Once the AED corrected that rhythm, his heart could pump again.
The blockage still needed clearing, of course, but since his heart could provide blood flow to critical organs, there was more time. And he had the safety of being under medical supervision.
***
As you’d expect, some of the world’s top cardiologists dropped everything to care for the AHA president.
Dr. Rose Marie Robertson, the AHA’s Chief Science and Medical Officer, caught up to John’s stretcher and got a quick report from the EMTs as they were getting on the elevator at the hotel. A glimpse of a normal heart rhythm on the portable monitor was reassuring. While following the ambulance in an Uber, she called Dr. Elliott Antman, a former AHA president and the author of the guidelines for treating STEMIs. Robertson and Antman were among the first to see John in the emergency room. Dr. James de Lemos, who helps run the cardiology program at John’s hospital, joined them. John’s predecessor and successor as AHA president stepped in to cover John’s other roles, as did AHA CEO Nancy Brown.
But here’s the great thing: No strings had to be pulled. John was saved because of systems in place to ensure every patient is cared for properly.
- His daughter started CPR immediately; immediate bystander CPR can make a big difference.
- He very rapidly got high-quality CPR from experts, because professionals who happened to be nearby had been trained to deliver it.
- He was defibrillated early with an AED because the hotel had one and promptly delivered it.
- Lauren’s 911 call set off Orange County’s chain of survival that connects emergency dispatchers, EMTs and the hospital emergency department. Seamless coordination doesn’t just happen. John knows this well because he oversaw the creation of a similar system(link opens in new window) while on the local AHA board in Dallas.
How effective all this can be was evident even that morning. While in the Emergency Department at University of California, Irvine Medical Center, John already wanted to talk with his family about items on his to-do list.
“I’m not going to be able to give my speech,” John said, referring to his presidential address. The cardiac arrest had transiently erased the memory of his compelling delivery of his talk – one that everyone agreed was spellbinding.
“You already gave it,” Lisa said.
“I did?!” John said. “Well, how’d I do?”
The comic delivery of that line — punctuated with a sly smile and self-deprecating chuckle — made it clear that John was already returning to form.
The final step in his chain of survival came in the catheterization lab.
Dr. Pranav Patel threaded a catheter into John’s right wrist and slid it to the troublesome spot. He then opened the artery and inserted a stent, a tube-like device that propped the artery open. John knows a lot about this, too. It’s a procedure he’s performed thousands of times.

Eventually, John got the whole story and reviewed his own films.
A single blocked artery did all this. Now that artery had a stent in it. Blood flow to that part of his heart was restored.
“Perfect,” he thought, his interventional cardiology background kicking in. “This seems very manageable.”
***
Once the moment-to-moment drama eased, Lisa, Jacob and Lauren began processing what happened.
They realized how differently things might’ve gone had they hustled downstairs for their ride to Pepperdine. Or if they hadn’t been there at all. In just the months since becoming AHA president, John had made a dozen trips across the country and around the world without them.
They racked their brains for warning signs they might’ve missed. They found none.

John refused to let his mind wander in those directions. In the hospital, he focused on “overwhelming gratitude” for his lifesavers and caregivers.
The gravity of how close he came to dying – no, to the fact he was dead for several minutes – hit once he was home in Dallas. Tears flowed hearing the emotion in the voices of family and friends.
“It still seems kind of surreal,” he said recently.
Although his ribs are still sore – probably broken; he hasn’t checked – he is back at work as both CEO of his hospitals and president of the AHA. He’s even in the early stages of crafting another speech for another AHA meeting, once again in Southern California. And even though his heart function is now normal, his top priority is cardiac rehab every Monday, Wednesday and Thursday.
John and Lisa have discussed doing all they can to track his risk for further cardiac events and to do all they can to deal with them meticulously. He’s focusing even more on improving his nutrition, keeping his exercise routine as a priority on his busy schedule and being even more careful about controlling the health factors we know are important.
They’ve also talked about “turning down the volume” on their lives. He defines that as filtering priorities through the question of what really matters.
***
In retrospect, several lines from John’s presidential address resonate louder.
Like the part where he talked about there being “no old men on either side of my family. None. All the branches of our family tree cut short by cardiovascular disease.”
And when he lamented how his father lived a far healthier lifestyle than his father, only to wind up needing bypass surgery at about the same age: “People like my dad remain a question.”

Now John has questions about himself, too.
If someone his age and with his variables had gone for a checkup, doctors wouldn’t have considered him at high risk. Yet, clearly, he was. If the pieces hadn’t fallen in place so perfectly, he’d be dead.
“There’s obviously something different about me,” he said. “Even if I think I have everything under control, the slot machine might still line up again.”
So, what can he do to prevent it? How can he tilt the odds in his favor?
Remember, he’s the CEO of a hospital system and the president of the American Heart Association. If the answers are out there, he can get them.
The problem is, they may not all be out there.
At least not yet.
For as much as we’ve learned about heart disease, there are still things we don’t know. Researchers continue mining for deeper insights, seeking ways to help the people on the ends of the bell curve, not just those in the middle.

View text version of infographic
“There’s this unknown of what more I could change,” John said. “But I remind myself that it wasn’t that long ago that we began to understand the role of cholesterol and high blood pressure in heart disease. There’s another breakthrough out there. Science will find it.”
Until then, the man whose presidential address was titled “Amplifying the Voice of Patients” is now a patient. Like his dad, he’s among more than 92 million Americans living with some form of cardiovascular disease or the after-effects of stroke.
“I always tell my heart attack patients you can’t change your parents – your genes are your genes – but you can work on what we know has proven to reduce your risk of this happening again,” John said. “That’s what I’ll do until we figure out the rest of this puzzle.”
***
Editor’s note: Dr. John Warner decided to share his story in hopes of inspiring others and raising awareness.

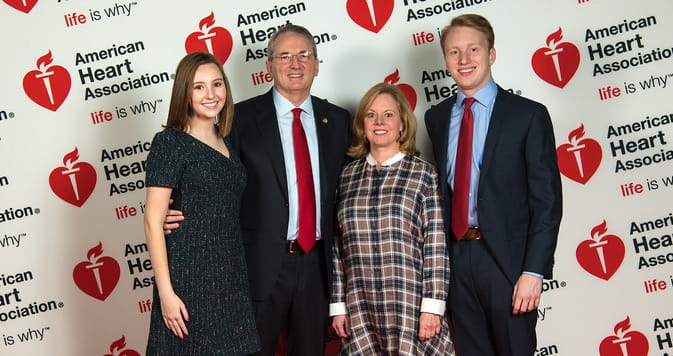
Lisa Warner and son Jacob Warner. (Photo by American Heart Association)





